Insulin Resistance in PCOS and Diabetes
Type 2 Diabetes (T2D) is an increasingly common health challenge affecting millions of people across the globe. Most people think of diabetes in terms of blood sugar which is usually the main focus of treatment. However, most people with the condition have dyslipidaemia or high cholesterol. The typical picture is one of low "good" cholesterol (HDL-C) and high "bad" cholesterol (LDL-C). If left untreated, this puts sufferers at risk of long-term health problems. To a lesser extent, many women with PCOS share this altered lipid profile and have insulin resistance.
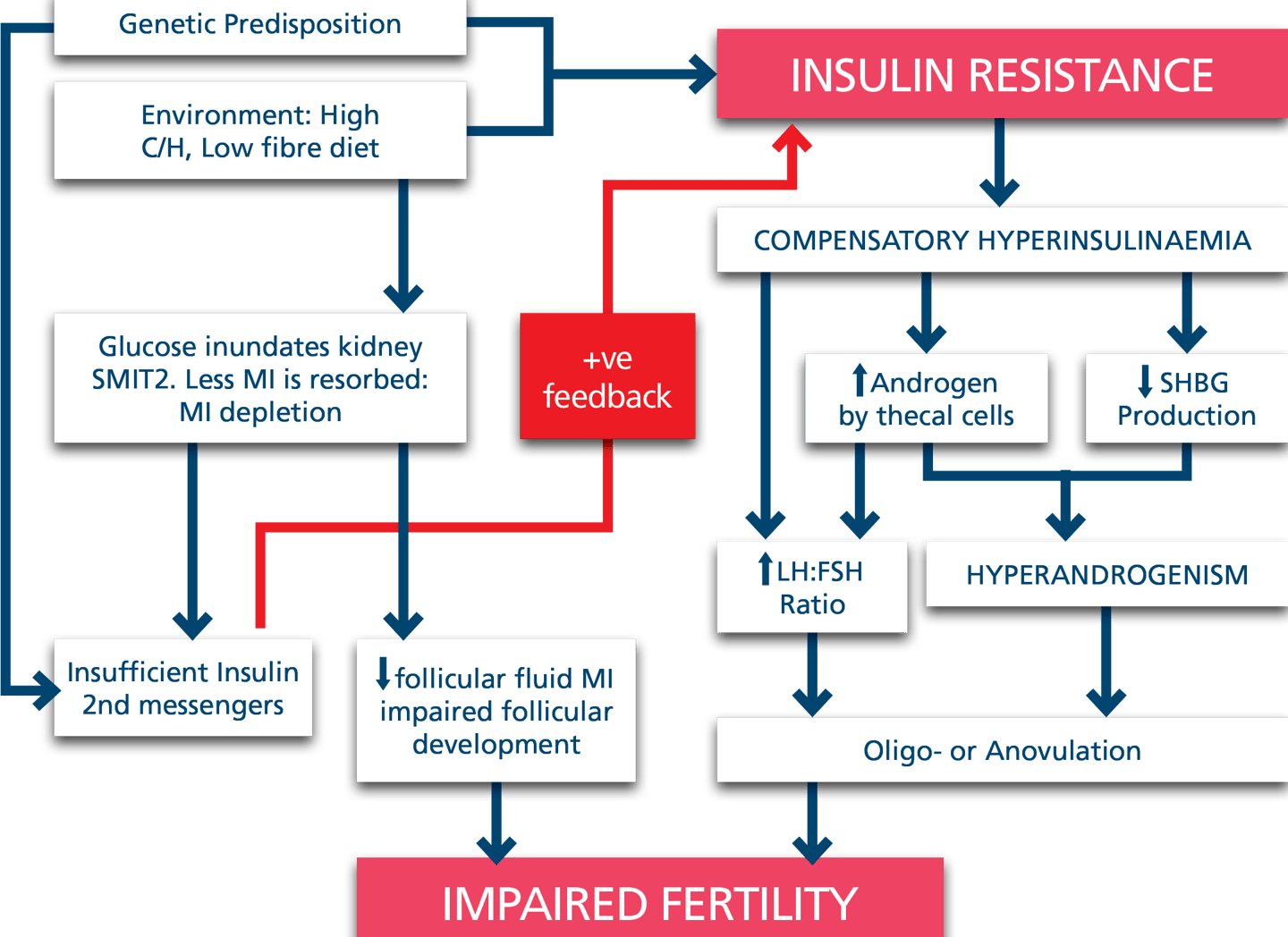
What causes insulin resistance in PCOS and T2D?
Insulin resistance is a shared feature of both conditions, the insulin is normal, the receptors are normal but the responsiveness to insulin is muted. For insulin to exert its actions it activates a number of other mediators known as 2nd messengers. At least 5 of these are made from inoself's active ingredient, myo-inositol NF12 and lipid regulation also relies on another regulatory molecule, phosphatidylinositol. If the body has an insufficient supply of these building blocks, the cells can not respond in the normal way.
It has been known for over 150 years that people with diabetes excrete much more inositol than normal. More recently, a similar finding has been observed among women with PCOS and among pregnant women who will go on to develop diabetes in pregnancy. The chemical structure of the active ingredient is similar to glucose and glucose is a precious energy source which is reabsorbed by the kidneys as it passes through. If someone has a genetic predisposition to PCOS and/or T2D they will have a tendency to develop high blood sugar. Similarly, if we have too much sugar in our diets (in refined sugar, fruit juices, smoothies or starchy foods), this can lead to a loss of myo-inositol - the very substrate that we need to be able to handle high sugar loads. A vicious cycle can develop and the conditions will become apparent.
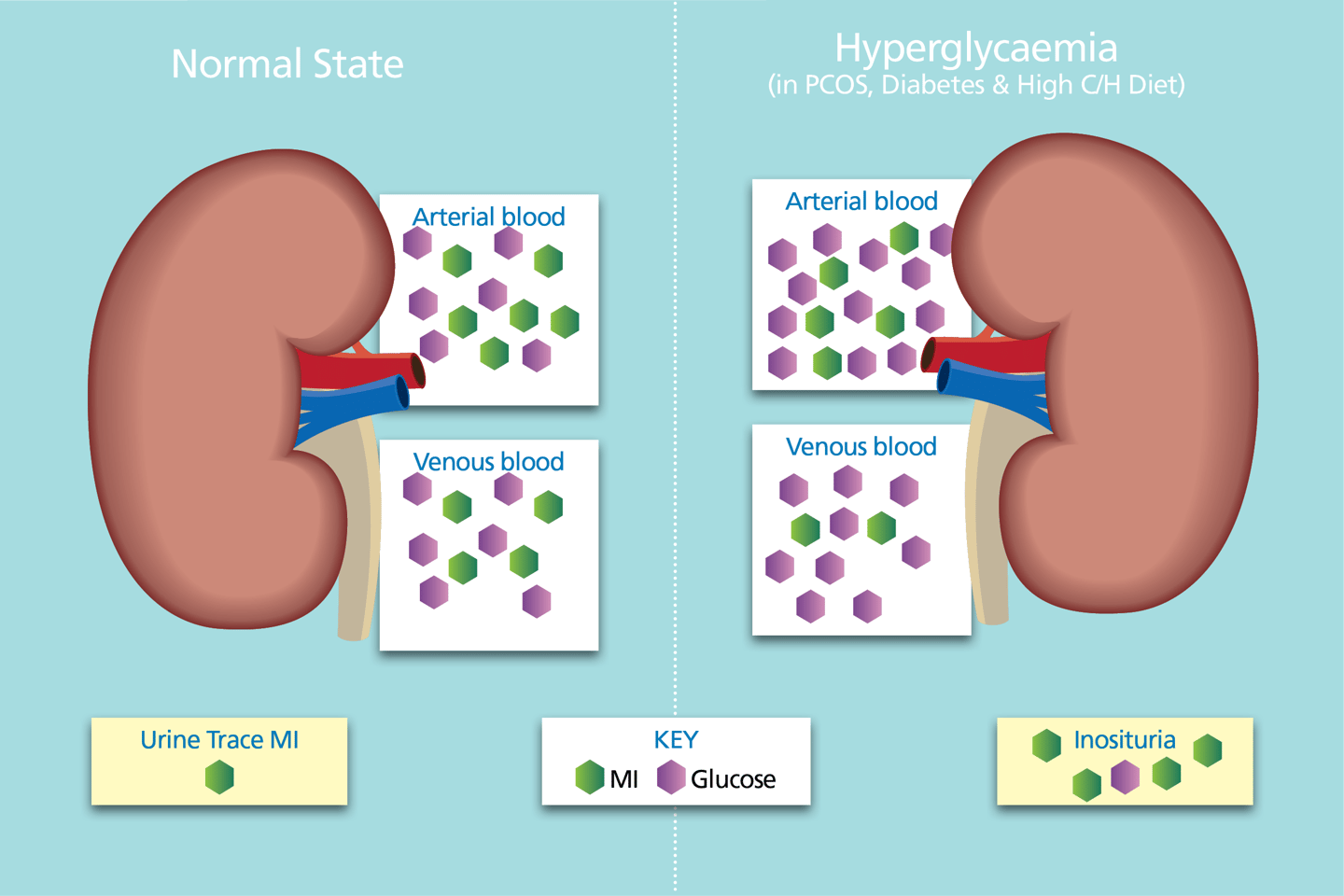
Glucose is a precious resource - maintaining circulating glucose is a priority.
In hyperglycaemia, SMIT2s become inundated with glucose thereby reducing the reabsorption capacity of SMIT2 activity for myo-inositol reabsorption.
More myo-inositol is excreted as a result.
In T2D and PCOS, urinary myo-inositol is typically 4-6x & 2-3x higher than the normal state. (6,7,8,9)
Arterial blood is filtered by the kidneys.
Almost 100% of glucose and myo-inositol enter the filtrate - both are actively reabsorbed.
Under normoglycaemic conditions, the activity levels of the sodium myo-inositol transport type 2 (SMIT2) co-transporters is normal and ≈100% is reabsorbed.
How can Replenitol help?
Replenitol works in two ways: it helps to regulate blood sugar, lowering it to normal levels and corrects the dyslipidaemia, also returning cholesterol to normal. It is the only treatment that can return your cholesterol to normal by elevating the "good" HDL component and lowering the "bad" LDL and triglyceride components. Typically, one sees a rise of 20% in HDL, a 20% reduction in LDL and a 35% reduction in triglycerides. Statins, by contrast, move cholesterol by 5-15% either raising both good and bad cholesterol or lowering both. Statins are not discriminatory and many who take them experience significant side effects.
Who should take Replenitol?
In Italy, this treatment has been used very successfully for more than 15 years. We are in the process of introducing it to the UK and Ireland. As it has no side effects and replaces a metabolite that most people with diabetes and PCOS lack, you can take the recommended dose of 4 tablets per day.